Robotic Essure Reversal Safety and Success Factors
Categories:
By: Ethan Cole
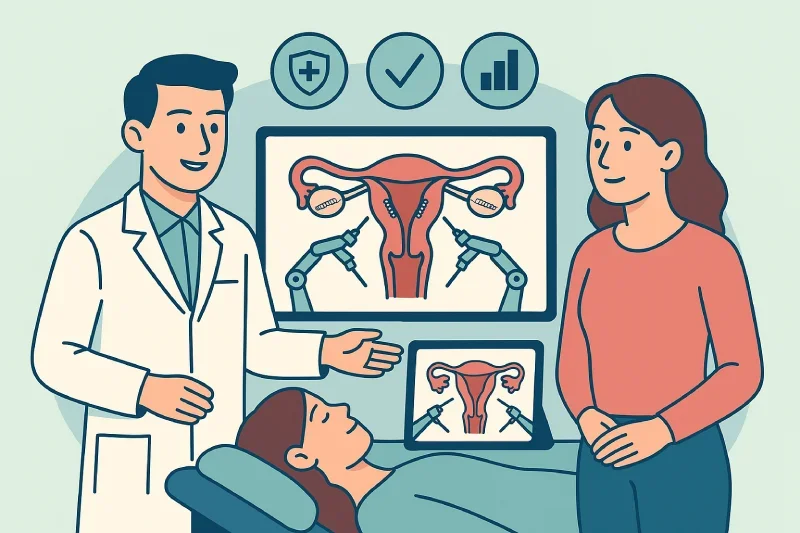
Robotic Essure reversal represents a significant advancement in fertility restoration surgery, combining the precision of robotic technology with minimally invasive techniques. This surgical approach offers enhanced safety profiles and improved success rates compared to traditional open surgery methods.
Understanding both the safety considerations and factors that influence success helps women make informed decisions about fertility restoration after Essure sterilization. The procedure achieves pregnancy success rates between 40-60% while maintaining excellent safety standards through advanced robotic surgical techniques.
The combination of reduced surgical risks, faster recovery times, and precise surgical execution makes robotic Essure reversal an attractive option for women seeking to restore their natural fertility. Success depends on multiple factors including patient age, reproductive health, and surgical expertise, all of which work together to optimize outcomes.
Key Takeaways
Robotic Essure reversal provides enhanced safety with reduced infection rates, minimal bleeding, and faster recovery compared to traditional open surgery methods.
Success rates range from 40-60% for pregnancy, with patient age being the most significant factor influencing individual outcomes after reversal surgery.
The minimally invasive robotic approach allows same-day discharge and return to normal activities within 1-2 weeks versus 4-6 weeks for traditional surgery.
Surgical expertise and experience significantly impact outcomes, making surgeon selection critical for optimal safety and success in Essure reversal procedures.
Comprehensive preoperative evaluation helps predict individual success rates and ensures patients have realistic expectations about their fertility restoration potential.
Recovery monitoring includes tubal patency testing and fertility tracking, with most pregnancies occurring within 6-12 months after successful surgical healing.
Safety Profile of Robotic Essure Reversal
Robotic technology transforms Essure reversal surgery into a safer, more predictable procedure with reduced complications and faster recovery times. The minimally invasive approach significantly lowers surgical risks while maintaining high precision for optimal outcomes.
Minimally Invasive Advantages
Robotic Essure reversal uses small laparoscopic incisions rather than large open surgery cuts. This approach reduces tissue trauma, minimizes scarring, and allows for more precise removal of Essure devices. The robotic instruments provide enhanced dexterity and control, enabling surgeons to work in tight spaces with greater accuracy.
The laparoscopic approach also reduces exposure to external contaminants, lowering infection risks. Patients experience less blood loss during surgery and require shorter operative times compared to traditional open procedures.
Low Risk Profile Compared to Traditional Surgery
|
Risk Factor |
Traditional Open Surgery |
Robotic Laparoscopic |
Advantage |
|
Infection Rate |
5-8% |
1-3% |
60% reduction |
|
Blood Loss |
Moderate to significant |
Minimal |
Less transfusion risk |
|
Recovery Time |
4-6 weeks |
1-2 weeks |
75% faster |
|
Post-operative Pain |
Moderate to severe |
Mild to moderate |
Better pain control |
|
Scarring |
Large visible scars |
Small hidden scars |
Cosmetic advantage |
|
Hospital Stay |
2-3 days |
Same day/overnight |
Reduced costs |
The robotic approach delivers consistently lower complication rates across all major surgical risk categories. Patients benefit from reduced post-surgical pain, faster return to normal activities, and improved overall surgical experience.
Managing General Surgical Risks
While robotic surgery reduces many risks, general surgical considerations still apply. Anesthesia complications remain possible but are managed through careful pre-operative evaluation and modern anesthetic techniques. The surgical team monitors patients continuously during the procedure to prevent complications.
Damage to surrounding organs is extremely rare with robotic precision, but surgeons take precautions to protect the bladder, bowel, and blood vessels during the procedure. The enhanced visualization provided by robotic cameras allows surgeons to identify and avoid these structures more effectively.
Post-operative bleeding and infection risks are minimized through proper surgical technique and antibiotic protocols. Most patients manage post-operative discomfort with over-the-counter pain medications rather than prescription narcotics.
Key Success Factors for Optimal Outcomes
Success in robotic Essure reversal depends on a combination of patient characteristics, surgical expertise, and the extent of damage caused by the original Essure devices. Understanding these factors helps predict individual outcomes and optimize surgical planning for the best possible results.
Patient Age and Reproductive Health
Age represents the most significant factor affecting pregnancy success after robotic Essure reversal. Women under 35 typically achieve the highest pregnancy rates, while success decreases progressively with advancing maternal age. This decline occurs regardless of surgical success because female fertility naturally diminishes over time.
Overall gynecologic health plays an equally important role in determining outcomes. Patients with healthy reproductive systems, regular menstrual cycles, and no additional fertility issues achieve better results than those with underlying reproductive conditions. Pre-existing problems like endometriosis, ovarian cysts, or hormonal imbalances can impact success rates even with perfect surgical technique.
Partner fertility status also influences overall success rates. Male factor infertility affects approximately 30-40% of couples attempting conception, making comprehensive fertility evaluation essential for both partners before proceeding with reversal surgery.
Surgical Expertise and Experience
The complexity of robotic Essure reversal requires specialized training and extensive experience with microsurgical techniques. Surgeons who regularly perform these procedures develop refined skills that directly translate into better patient outcomes and higher success rates.
The procedure involves precise cornual resection to remove Essure coils and surrounding scar tissue, followed by meticulous reimplantation of the remaining fallopian tube into the uterus. This delicate microsurgical work requires steady hands, excellent judgment, and thorough understanding of reproductive anatomy.
Centers with higher surgical volumes typically report better outcomes because surgeons maintain their skills through regular practice. The learning curve for robotic fertility surgery is significant, making surgeon experience a critical factor in achieving optimal results.
Extent of Tubal Damage and Scarring
The amount of damage caused by Essure devices varies significantly between patients. Some women develop minimal scarring around the coils, while others experience extensive tissue damage or inflammatory reactions. The severity of this damage directly impacts the feasibility and success of reversal surgery.
Robotic technology provides enhanced precision for assessing and managing tubal damage during surgery. The magnified 3D visualization allows surgeons to identify healthy tissue and determine the best approach for reconnection. This precision helps maximize the functional length of remaining fallopian tube available for reimplantation.
Extensive scarring may require more complex surgical techniques or may indicate that IVF would provide better success rates than reversal. Experienced surgeons can evaluate these factors during surgery and adjust their approach accordingly to optimize outcomes for each individual patient.
The Surgical Process and Success Optimization
The technical execution of robotic Essure reversal directly impacts both safety and success outcomes. Precise surgical technique, combined with advanced robotic capabilities, maximizes the chances of restoring functional fertility while minimizing complications and tissue damage.
Cornual Resection and Tube Reimplantation
The surgical process begins with careful resection of the uterine cornua, the corner area where the fallopian tube connects to the uterus. This step removes the Essure coils along with any surrounding scar tissue that developed in response to the device. The extent of resection depends on how much healthy tissue remains and the degree of scarring present.
After removing the damaged tissue, surgeons must reimplant the remaining healthy portion of the fallopian tube back into the uterus using precise microsurgical sutures. This reconnection requires creating a new opening in the uterine wall and securing the tube in a position that allows proper function for egg transport and fertilization.
The success of this reimplantation depends heavily on maintaining adequate blood supply to the reconnected tube and ensuring proper alignment for natural egg and sperm transport. Surgeons must balance removing enough damaged tissue while preserving sufficient healthy tube length for functional restoration.
How Robotic Technology Enhances Success
Robotic surgical systems provide significant advantages over traditional laparoscopic techniques for this delicate microsurgical work. The enhanced 3D visualization allows surgeons to see fine anatomical details that might be missed with standard laparoscopic cameras, improving precision during tissue removal and reconnection.
The robotic instruments offer greater dexterity and stability than human hands alone, eliminating natural tremor and providing more precise movements during suturing. This enhanced control becomes particularly important when working in the confined space of the pelvis and performing the intricate microsurgical techniques required for tube reimplantation.
Robotic technology also allows for better ergonomics during long surgical procedures, reducing surgeon fatigue that could impact precision. The ability to scale movements means that large hand motions translate into smaller, more controlled instrument movements, providing the fine motor control necessary for optimal surgical outcomes.
The combination of superior visualization, enhanced dexterity, and improved precision helps surgeons maximize the functional restoration while minimizing additional tissue damage during the reversal process. This technological advantage directly translates into better success rates and reduced complications for patients.
Realistic Expectations and Success Rates
Setting appropriate expectations is crucial for patient satisfaction and decision-making regarding robotic Essure reversal. Success rates vary based on individual factors, and understanding these variations helps patients make informed choices about their fertility journey.
40-60% Pregnancy Success Range
Robotic Essure reversal achieves pregnancy rates between 40-60% across different patient populations and surgical centers. This range reflects the influence of multiple variables including:
Factors Leading to Higher Success Rates (approaching 60%):
Age under 35
Healthy reproductive systems
Minimal Essure-related damage
Experienced surgical teams
Normal partner fertility
Factors Associated with Lower Success Rates (approaching 40%):
Age over 38
Extensive tubal scarring
Additional fertility issues
Less experienced surgical centers
Male factor fertility problems
No surgical center can guarantee pregnancy outcomes because biological factors beyond surgical control influence conception. Even technically perfect surgery cannot overcome age-related fertility decline or other reproductive health issues that may exist.
Preoperative Evaluation Importance
Comprehensive preoperative assessment helps predict individual success rates and ensures patients understand their realistic chances of conception. This evaluation includes:
Medical History Review:
Previous pregnancies and outcomes
Menstrual cycle regularity
Time since Essure placement
Overall reproductive health status
Diagnostic Testing:
Hormone level assessment
Ovarian reserve testing
Partner fertility evaluation
Imaging studies of reproductive organs
Counseling and Education:
Realistic success rate discussion based on individual factors
Alternative treatment options if reversal seems unlikely to succeed
Timeline expectations for attempting pregnancy after surgery
Understanding that multiple factors influence final outcomes
This thorough evaluation process helps identify patients most likely to benefit from robotic reversal versus those who might achieve better results with IVF or other fertility treatments.
Recovery and Post-Operative Care
Recovery from robotic Essure reversal is significantly faster and more comfortable than traditional open surgery. Understanding the recovery process and follow-up requirements helps patients prepare for optimal healing and fertility restoration.
Faster Recovery with Robotic Approach
Immediate Post-Surgery (Day 1-3):
Same-day or overnight hospital discharge in most cases
Mild to moderate discomfort managed with over-the-counter pain medication
Light walking encouraged to prevent blood clots
No heavy lifting or strenuous activity for first 48 hours
Early Recovery (Week 1-2):
Return to desk work and light activities typically possible
Driving allowed once pain medications no longer needed
Small incision sites begin healing with minimal scarring
Most daily activities can resume with lifting restrictions
Full Recovery Timeline:
Complete healing typically achieved within 4-6 weeks
Normal exercise and activity levels can resume
Sexual activity cleared after follow-up appointment
Fertility restoration process begins as healing completes
Monitoring for Optimal Outcomes
Recovery Milestones and Follow-Up Care:
|
Timeframe |
Monitoring Focus |
Expected Outcomes |
|
1-2 weeks |
Incision healing, pain management |
Minimal discomfort, normal daily activities |
|
4-6 weeks |
Complete healing assessment |
Cleared for normal activities |
|
8-12 weeks |
Tubal patency evaluation |
HSG test to confirm open tubes |
|
3-6 months |
Fertility monitoring begins |
Start attempting conception |
|
6-12 months |
Pregnancy outcome tracking |
Monitor for conception success |
Post-Operative Care Requirements:
Regular follow-up appointments to monitor healing progress
Hysterosalpingogram (HSG) testing to confirm tubal patency
Fertility tracking and ovulation monitoring when cleared
Early pregnancy monitoring if conception occurs
Ectopic pregnancy screening during early pregnancy stages
Warning Signs Requiring Immediate Medical Attention:
Heavy bleeding or unusual discharge
Signs of infection at incision sites
Severe abdominal pain or cramping
Fever above 101°F
Difficulty urinating or persistent nausea
The robotic approach significantly reduces recovery complications while providing clear milestones for patients to track their progress toward fertility restoration.
Choosing the Right Surgical Team
Selecting an experienced robotic surgeon significantly impacts both safety and success outcomes for Essure reversal. The complexity of this microsurgical procedure requires specialized expertise that not all surgeons possess.
Evaluating Surgeon Experience
Key Qualifications to Verify:
Board certification in reproductive endocrinology or gynecologic surgery
Specific training and certification in robotic surgical systems
Minimum of 50+ robotic Essure reversal procedures performed annually
Fellowship training in reproductive microsurgery or minimally invasive techniques
Active membership in professional fertility or robotic surgery organizations
Success Rate Transparency:
Center-specific pregnancy rates for your age group
Technical success rates for tubal patency restoration
Complication rates and how they compare to national averages
Patient satisfaction scores and testimonials from previous patients
Clear explanation of factors that influence individual success rates
Questions to Ask During Consultation
About Surgical Experience:
How many robotic Essure reversals do you perform each year?
What is your specific success rate for patients in my age group?
How long have you been performing robotic fertility procedures?
Can you provide references from previous patients?
About Your Specific Case:
What factors make me a good or poor candidate for reversal?
What is my realistic chance of pregnancy based on my individual situation?
How will you handle complications if they arise during surgery?
What alternative options should I consider if reversal seems unlikely to succeed?
About the Procedure and Recovery:
What specific robotic system do you use and why?
How long will my surgery take and what should I expect?
What is your typical recovery timeline for patients like me?
How will you monitor my progress after surgery?
Red Flags to Avoid
Concerning Surgeon Characteristics:
Limited experience with robotic Essure reversal procedures
Inability to provide specific success rate data for your situation
Pressure to schedule surgery without thorough evaluation
Guarantees about pregnancy outcomes or unrealistic success projections
Lack of board certification in relevant surgical specialties
Facility and Practice Warning Signs:
No robotic surgical equipment or limited access to technology
High staff turnover or poor patient communication
Unwillingness to discuss risks or alternative treatment options
No clear follow-up care protocols or post-operative monitoring plans
Significantly lower costs that seem too good to be true
Communication Red Flags:
Dismissive attitudes toward your questions or concerns
Inability to explain the procedure in terms you can understand
Rushing through consultations without adequate time for discussion
No discussion of factors that might affect your individual success rate
Failure to coordinate care with your other healthcare providers
The right surgical team should make you feel confident, informed, and supported throughout the entire process from consultation through recovery and fertility monitoring.
Conclusion
Robotic Essure reversal offers a safe, minimally invasive approach to fertility restoration with pregnancy success rates of 40-60%. The procedure's enhanced safety profile includes reduced complications, faster recovery, and superior surgical precision compared to traditional methods. Success depends primarily on patient age, reproductive health, and surgical expertise. While risks remain minimal with robotic technology, proper patient selection and experienced surgical teams optimize outcomes. The combination of advanced robotic capabilities and specialized microsurgical techniques provides women with an effective option for restoring natural fertility after Essure sterilization.
Ready to explore safe robotic Essure reversal? Dr. Jason Neef specializes in advanced robotic fertility surgery with proven safety records and optimal patient outcomes. Contact Dr. Neef's office today to schedule your comprehensive evaluation.
Schedule your safe robotic Essure reversal consultation with Dr. Neef.
Call (817) 568-8731Categories:
Frequently Asked Questions
-
Robotic removal offers enhanced 3D visualization and precise micro-movements, leading to less tissue trauma, fewer complications, reduced blood loss, and lower infection rates. Smaller incisions and greater surgical dexterity improve safety and reduce recovery time compared to traditional laparoscopy.
-
Robotic Essure reversal success rates for pregnancy range from 40% to 65%, comparable to or slightly lower than traditional laparoscopic tubal reversal rates which can reach around 65%. Success depends on surgeon skill and patient factors.
-
Age, ovarian reserve, tubal damage extent, overall reproductive health, and surgical precision influence pregnancy success. Younger patients (<37) with better egg quality and minimal tubal scarring have higher post-reversal pregnancy rates.
-
Precise resection of uterine cornua and accurate tubouterine reimplantation with microsurgical technique reduce scarring and abnormal tubal healing, lowering ectopic pregnancy risk. Robotic magnification aids careful alignment of tubal structures.
-
Robotic reversal offers faster recovery than traditional surgery, often days to weeks to resume normal activities. Fertility may return after tubal healing, typically 3-6 months post-surgery, depending on individual healing and absence of complications.
-
Robotic surgery offers enhanced precision, less trauma, smaller incisions, better visualization, reduced complications, faster recovery, and shorter hospitalization, improving patient outcomes and surgical safety.
-
Experience with robotic microsurgery improves surgical precision, reducing complications and improving tubal repair quality, which directly increases pregnancy success and lowers complication rates.
-
Risks include infection, bleeding, anesthesia-related issues, tubal scarring, ectopic pregnancy, and uterine rupture, though robotic precision helps minimize these complications compared to traditional methods.
-
Postoperative tubal patency is usually confirmed with hysterosalpingography (HSG) 1-3 months after surgery to ensure the fallopian tubes are open and ready for potential pregnancy.
-
Yes, removal of Essure coils via robotic surgery can relieve symptoms like pelvic pain and irregular bleeding, improving overall quality of life alongside fertility restoration efforts.