Robotic Hysterectomy Surgical Precision Explained
Categories:
By: Ethan Cole
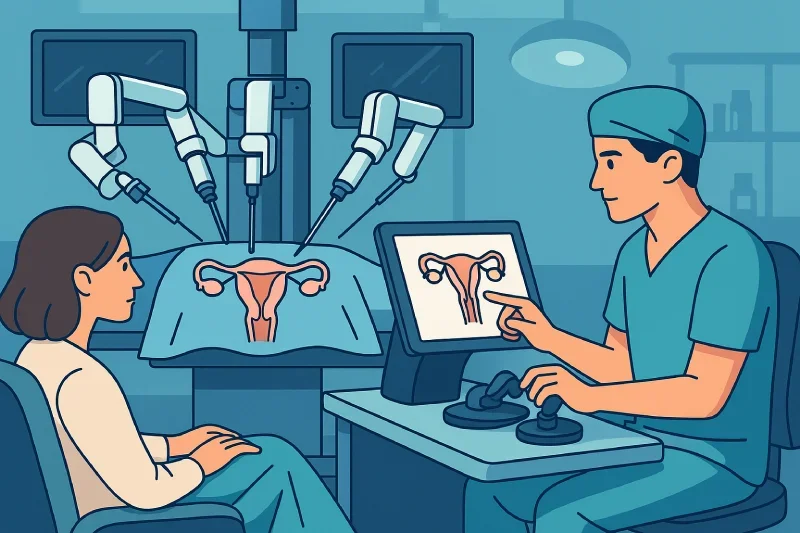
A hysterectomy—the surgical removal of the uterus—is one of the most commonly performed gynecologic procedures. In the past, this operation often required large abdominal incisions, extended hospital stays, and lengthy recoveries. But today, thanks to advances in surgical technology, many patients can benefit from a far less invasive option: robotic-assisted hysterectomy.
Robotic hysterectomy uses small incisions and computer-enhanced instruments to help surgeons perform precise, complex procedures with improved accuracy and control. This technique allows for reduced pain, shorter recovery time, and fewer complications compared to traditional open surgery.
In this guide, we’ll explain how robotic hysterectomy works, when it’s medically recommended, what to expect before and after surgery, and how it compares to other surgical methods. Whether you’re facing a gynecologic condition or exploring treatment options, understanding this modern surgical approach can help you make an informed decision with your healthcare provider.
Key Takeaways
Robotic hysterectomy offers minimally invasive precision with smaller incisions, less pain, and faster recovery than open surgery, making it an effective option for many gynecologic conditions.
This procedure is particularly beneficial for women with large fibroids, pelvic adhesions, obesity, or prior surgeries, where visualization and delicate surgical control are essential for safe outcomes.
Compared to traditional hysterectomy, robotic-assisted surgery reduces blood loss, hospital stays, and recovery time, with most patients returning to light activities within 2–3 weeks.
While robotic hysterectomy is safe, risks include bleeding, infection, anesthesia reactions, or organ injury—though complication rates are generally lower than open abdominal procedures.
Surgeon experience with the da Vinci system directly impacts outcomes, with higher case volume linked to fewer complications, shorter operative times, and more successful recoveries.
Costs are higher than laparoscopic or vaginal hysterectomy due to advanced equipment, but shorter recovery and reduced complications may offset long-term expenses.
Robotic hysterectomy is often chosen for both benign conditions and early-stage gynecologic cancers, offering enhanced precision for complex dissections and lymph node removal.
Recovery typically involves same-day or overnight discharge, with full healing in 4–6 weeks, supported by gradual return to activity and close follow-up care with the surgeon.
What Is a Robotic Hysterectomy?
A robotic hysterectomy is a modern, minimally invasive procedure used to surgically remove the uterus. It is performed using advanced robotic technology that allows the surgeon to operate through a few small incisions with enhanced precision and control. This approach is often chosen for its lower risk of complications, quicker recovery, and suitability for more complex gynecologic conditions.
Definition and Overview of the Procedure
Robotic hysterectomy involves the removal of the uterus using robotic-assisted instruments controlled by a surgeon. The goal of the procedure may be to treat conditions like uterine fibroids, endometriosis, abnormal bleeding, or even early-stage cancer. In some cases, the cervix, ovaries, or fallopian tubes may also be removed during the surgery, depending on the patient’s medical needs.
Unlike traditional open surgery, which requires a large abdominal incision, robotic hysterectomy is performed through several small incisions in the lower abdomen. This technique is part of the broader category of minimally invasive surgery.
How Robotic-Assisted Surgery Works
During the procedure, the surgeon sits at a console and uses hand and foot controls to manipulate robotic arms that hold surgical instruments. These instruments offer a greater range of motion than the human hand and allow for extremely precise movements.
The system provides a magnified, high-definition 3D view of the surgical field, enabling the surgeon to see and work with fine detail. Despite the term "robotic," the robot does not act on its own—the surgeon is in complete control at all times.
How It Differs from Traditional and Laparoscopic Methods
Robotic hysterectomy shares some similarities with laparoscopic surgery but offers several distinct advantages:
Smaller incisions than open surgery, which means less visible scarring
Greater range of motion and control compared to standard laparoscopic tools
Better 3D visualization, improving accuracy during delicate procedures
Reduced risk of bleeding, infection, and tissue trauma
Shorter hospital stays and faster return to daily activities
While robotic hysterectomy may not be necessary for every patient, it’s particularly valuable for those with complex anatomy, large fibroids, or prior pelvic surgeries.
When Is Robotic Hysterectomy Needed?
Robotic hysterectomy is not always the first treatment option for gynecologic issues. However, it becomes a highly effective and appropriate solution when less invasive approaches fail or when certain conditions require surgical removal of the uterus. Its precision and minimally invasive nature make it especially useful in cases where traditional surgery may carry higher risks.
Common Conditions Treated with Robotic Hysterectomy
Several gynecologic conditions may lead a healthcare provider to recommend a hysterectomy, and robotic-assisted surgery can be the preferred approach for:
Uterine fibroids – Noncancerous growths that cause pelvic pain, pressure, or heavy menstrual bleeding
Endometriosis – Painful tissue growth outside the uterus that may be resistant to medication
Uterine prolapse – When the uterus drops into the vaginal canal, causing discomfort or urinary issues
Abnormal uterine bleeding – Especially when unresponsive to hormone therapy or other treatments
Early-stage gynecologic cancers – Such as uterine, cervical, or ovarian cancer, where complete removal is medically indicated
The robotic platform allows for delicate dissection and precision during these complex procedures, improving outcomes and reducing surgical trauma.
Complex Surgical Cases That Benefit Most
Robotic hysterectomy is particularly beneficial in more challenging surgical situations, such as:
Large or irregularly shaped uterus
Extensive pelvic adhesions from prior surgeries or infections
Coexisting conditions like obesity, which may complicate open or standard laparoscopic procedures
Anatomical abnormalities or deep infiltrating endometriosis
In these scenarios, the enhanced visualization and precise movement of robotic instruments can reduce the risk of complications and improve surgical success.
When Less Invasive Options Have Failed
In many cases, hysterectomy is considered only after other treatments—like hormonal therapy, IUD placement, or minimally invasive uterine procedures—have failed to resolve symptoms. Robotic hysterectomy offers a next-level option for patients who need definitive treatment but want to avoid the long recovery and risks of open abdominal surgery.
How the Procedure Works: Step-by-Step
Understanding what happens before, during, and after robotic hysterectomy can help patients feel more prepared and confident. While the technology is advanced, the process itself is highly structured and patient-focused.
Preoperative Preparation and Planning
Before the procedure, you’ll meet with your gynecologic surgeon to review your medical history, discuss your surgical goals, and ensure you’re a good candidate for robotic hysterectomy. Preparation may include:
Pelvic exam and ultrasound imaging
Blood tests to assess overall health
Review of any medications that may need to be paused before surgery
Instructions on fasting, bowel preparation, or hygiene before the procedure
You’ll also be informed about the anesthesia process, surgical risks, and what to expect during recovery.
Surgical Process Using the Robotic System
On the day of surgery, you’ll receive general anesthesia to ensure comfort and safety. The procedure typically follows these steps:
Small incisions (usually 3–5) are made in the lower abdomen
Trocar ports are inserted to allow access for robotic instruments
The robotic system is docked to the ports and the surgeon begins the operation
Using a console, the surgeon controls robotic arms equipped with precise surgical tools
The uterus is carefully detached from surrounding tissues and blood vessels
Depending on the case, the cervix, ovaries, or fallopian tubes may also be removed
The uterus is extracted through the vagina or via one of the abdominal incisions
The area is checked for bleeding, instruments are removed, and incisions are closed
The entire procedure generally takes 1.5 to 3 hours, depending on complexity.
Role of the Surgeon and Robotic Console
Despite the name, the robot does not perform the surgery on its own. The surgeon is in complete control, operating from a specialized console a few feet away from the patient. The console offers:
A high-definition, 3D magnified view of the surgical area
Hand and foot controls to guide each robotic arm with exceptional accuracy
Tools that rotate and bend beyond the range of the human wrist
This technology allows for greater precision, better visualization, and more delicate handling of tissues than standard laparoscopic or open techniques.
Benefits of Robotic Hysterectomy
Robotic hysterectomy has become a preferred option for many patients and surgeons due to its combination of minimally invasive technique and advanced surgical precision. Compared to traditional open or standard laparoscopic approaches, robotic-assisted surgery offers multiple benefits across both clinical outcomes and patient recovery.
Reduced Blood Loss and Infection Risk
Because robotic surgery uses smaller incisions and provides more refined control, patients often experience significantly less blood loss during the procedure. This decreases the need for transfusions and lowers the risk of postoperative infections. The precise dissection also minimizes damage to surrounding tissues, contributing to faster healing.
Smaller Incisions, Less Pain, and Faster Recovery
The incisions made during robotic hysterectomy are typically only 0.5 to 1 cm in size. This translates to:
Minimal postoperative discomfort
Reduced need for strong pain medications
Shorter hospital stays (often same-day or overnight)
Faster return to normal daily activities—usually within 2 to 3 weeks
Patients also experience fewer wound-related complications, such as hernias or prolonged scarring.
Improved Surgical Precision for Complex Cases
Robotic systems are especially valuable in surgeries involving:
Large fibroids or bulky uterus
Extensive pelvic adhesions from prior surgeries
Endometriosis involving other pelvic structures
Obesity, which can limit visibility and access in traditional methods
The enhanced 3D vision and wristed instruments allow the surgeon to perform delicate maneuvers with better outcomes, even in anatomically challenging situations.
Comparison of Surgical Approaches
|
Feature |
Robotic Hysterectomy |
Laparoscopic Hysterectomy |
Open Hysterectomy |
|
Incision Size |
0.5–1 cm |
0.5–1 cm |
10–15 cm |
|
Blood Loss |
Minimal |
Moderate |
Higher |
|
Pain Level |
Low |
Moderate |
High |
|
Hospital Stay |
Same-day to 1 night |
1–2 nights |
2–4 nights |
|
Recovery Time |
2–3 weeks |
3–4 weeks |
6–8 weeks |
|
Complication Risk |
Lower |
Moderate |
Higher |
|
Precision in Complex Cases |
High |
Moderate |
Moderate |
Robotic vs Other Hysterectomy Techniques
There are several surgical options available for performing a hysterectomy, and each method comes with its own benefits and limitations. Robotic hysterectomy is one of the most advanced techniques, but laparoscopic and open (abdominal) procedures may still be appropriate depending on the patient’s condition, anatomy, and surgical history.
Key Differences in Technique and Outcomes
All three methods aim to remove the uterus, but the approach, instruments used, and recovery experience can vary significantly. Here's a direct comparison across the most important clinical and patient-focused factors:
|
Feature |
Robotic Hysterectomy |
Laparoscopic Hysterectomy |
Open (Abdominal) Hysterectomy |
|
Surgical Access |
Small incisions (robotic arms) |
Small incisions (manual tools) |
Large abdominal incision |
|
Visualization |
3D high-definition magnified view |
2D camera view |
Direct line of sight |
|
Instrument Precision |
High (wristed instruments) |
Moderate (rigid tools) |
Standard surgical tools |
|
Blood Loss |
Minimal |
Moderate |
Higher |
|
Pain and Discomfort |
Low |
Moderate |
High |
|
Hospital Stay |
Same-day or 1 night |
1–2 nights |
2–4 nights |
|
Recovery Time |
2–3 weeks |
3–4 weeks |
6–8 weeks |
|
Use in Complex Cases |
Excellent |
Limited |
Moderate to High |
Pros and Cons of Each Surgical Option
Robotic Hysterectomy
Pros: Superior precision, excellent for complex anatomy, quick recovery, less pain
Cons: Not available at all hospitals, higher equipment cost, may not be necessary for simple cases
Laparoscopic Hysterectomy
Pros: Minimally invasive, lower cost than robotic, widely available
Cons: Less precision, harder to use in complex or obese patients
Open Hysterectomy
Pros: Direct access for very large uteri or extensive disease
Cons: Longer recovery, more pain, higher risk of complications
Choosing the Right Method for Your Situation
The best surgical method depends on several factors, including your medical diagnosis, body type, surgical history, and overall health. Robotic hysterectomy is often preferred for patients with complex anatomy, significant adhesions, or obesity. However, simpler cases may be managed effectively with laparoscopic or even vaginal hysterectomy.
Ultimately, the right choice should be made in consultation with a skilled gynecologic surgeon who can evaluate your individual needs and explain all available options.
What to Expect During Recovery
Recovery from robotic hysterectomy is generally faster and more comfortable than recovery from traditional open surgery.
Most patients return home the same day or after a brief hospital stay and can resume light activities within a couple of weeks. While individual healing times may vary, knowing what to expect can help you prepare both physically and mentally.
Typical Recovery Timeline
First few days: Mild to moderate abdominal soreness, fatigue, and possible bloating or gas pains. Most patients can walk, eat, and perform basic tasks shortly after surgery.
Week 1–2: Gradual improvement in energy levels and reduced need for pain medication. Many people return to desk-based work or light activity.
Week 3–4: Most patients feel significantly better and can resume moderate exercise or daily routines with minimal discomfort.
By week 6: Full recovery is expected for most individuals, though your surgeon may advise waiting longer before engaging in heavy lifting or sexual activity.
Activity Restrictions and Pain Management
Avoid lifting anything over 10 pounds for at least 2 weeks
No strenuous exercise, running, or abdominal workouts for 4–6 weeks
Pain is usually managed with over-the-counter medications; narcotics are rarely needed
Driving is typically safe within a week, once pain medications are no longer required
Light walking is encouraged early to improve circulation and prevent blood clots
Always follow your specific discharge instructions, as recovery protocols can vary depending on your individual case and any additional procedures performed.
Postoperative Follow-Up and Healing Milestones
A follow-up appointment is typically scheduled within 1 to 2 weeks after surgery to monitor healing and address any concerns. During this visit, your surgeon may:
Examine your incisions
Review pathology results (if applicable)
Discuss next steps regarding hormone changes, if your ovaries were removed
Clear you for increased activity or return to work
You should contact your provider if you notice signs of infection, increasing pain, heavy bleeding, or unusual discharge.
Risks and Considerations of Robotic Hysterectomy
While robotic hysterectomy offers many advantages, it’s important to understand that every surgical procedure carries some level of risk. Knowing the potential complications and limitations can help you make an informed decision with your healthcare provider and set realistic expectations for recovery.
Potential Complications to Be Aware Of
Most patients experience a smooth recovery, especially when surgery is performed by a skilled and experienced team. However, complications can occur, including:
Bleeding during or after the procedure
Infection at the incision sites or internally
Injury to surrounding organs (e.g., bladder, ureters, intestines)
Blood clots (deep vein thrombosis or pulmonary embolism)
Adverse reactions to anesthesia
Ectopic tissue scarring or internal adhesions
Conversion to open surgery if complications arise mid-procedure (rare)
These risks are generally low with robotic-assisted surgery but still warrant discussion and monitoring.
When Robotic Surgery May Not Be Suitable
Robotic hysterectomy isn’t ideal for every patient. Some situations where it may not be the best option include:
Very large fibroids or extreme uterine enlargement that limits robotic access
Lack of available robotic equipment or trained surgeons at your facility
Certain cases of extreme obesity where visibility is still compromised
Cost concerns, as robotic surgery may not be fully covered by all insurance plans or may involve higher facility fees
In such cases, alternative surgical methods—such as laparoscopic, vaginal, or open abdominal hysterectomy—may be considered based on your anatomy and health status.
Emotional and Hormonal Aftereffects
In addition to physical healing, it’s important to recognize the emotional and hormonal changes that can occur after a hysterectomy:
Patients who have their ovaries removed may experience sudden menopause, with symptoms like hot flashes, mood swings, or sleep issues
Even when the ovaries remain intact, some individuals report emotional shifts, including sadness or a sense of loss
Fertility is permanently affected, which can be emotionally challenging, particularly for younger patients
Counseling, support groups, and hormonal therapy (if indicated) can help you manage these changes and navigate the adjustment process more comfortably.
Conclusion
Robotic hysterectomy is a powerful advancement in women’s health, offering greater precision, smaller incisions, less pain, and a faster recovery than traditional surgical options. It’s especially valuable for patients facing complex conditions like large fibroids, endometriosis, or prior pelvic surgeries. While every case is unique, this minimally invasive approach continues to expand access to safer, more effective uterine surgery.
For those considering their options, consultation with an experienced gynecologic surgeon is essential. Robotic surgery may not be necessary for every patient, but in the right hands, it can significantly improve outcomes and quality of life.
Dr. Jason Neef is a board-certified OB/GYN with extensive expertise in robotic-assisted gynecologic procedures. He specializes in tailoring treatment plans to meet each patient’s individual needs, ensuring that decisions are based on both advanced surgical techniques and compassionate, evidence-based care. Patients trust Dr. Neef for clear guidance and excellent outcomes.
Schedule your robotic hysterectomy consultation today.
Call (817) 568-8731Categories:
Frequently Asked Questions
-
The surgeon sits at a console and uses hand controllers to operate robotic arms. The system translates hand movements into precise micromovements with tremor filtering, ensuring steadiness and accuracy during surgery.
-
The 3D high-definition view provides magnified, detailed visualization of the surgical field with depth perception, allowing surgeons to clearly see fine anatomical structures for delicate dissections and suturing.
-
Robotic hysterectomy offers greater instrument dexterity and 3D visualization, leading to less blood loss, reduced tissue trauma, and faster recovery compared to traditional laparoscopic hysterectomies.
-
Unique risks include possible technical malfunctions, longer operative times during the learning curve, and issues from improper positioning or equipment failure, though overall complication rates remain low.
-
Future advances may include enhanced haptic feedback, smaller and more flexible instruments, AI-assisted surgeon guidance, and even greater precision and safety for complex gynecologic procedures.
-
Wristed instruments mimic human wrist movement with seven degrees of freedom, allowing surgeons to perform highly intricate movements not possible with standard laparoscopic tools.
-
Tremor filtration removes natural hand tremors, providing smooth, stable instrument movement that enhances accuracy during delicate surgical steps.
-
Patients usually experience less pain, smaller incisions, reduced blood loss, and faster return to normal activities compared to open or conventional laparoscopic surgery.
-
Patients with large uteri, obesity, extensive pelvic adhesions, or prior abdominal surgeries benefit most from robotic hysterectomy due to enhanced visualization and precision.
-
The console’s seated position reduces surgeon fatigue during long operations, improving focus and consistency, which may lead to better patient outcomes.